Bone grafting is an oral procedure that enables us to grow bone where needed and promote new bone growth where the jaw bone may be sparse or of poor quality due to atrophy. The bone structure in the jaw weakens over time if missing teeth are not replaced in a timely manner. This often leads to poor quality and quantity of bone, making the jaw unsuitable for the placement of dental implants. However, with a bone grafting procedure, Dr. Falender can repair this deficiency through a variety of treatments. Whether a bone graft is used to fix a single tooth site, a large area where multiple teeth have been lost, or a congenital defect, Indianapolis Oral Surgery & Dental Implant Center has a solution to restore your oral function and aesthetic appearance.
Why Do I Need a Bone Graft?
You Are Missing a Tooth or Multiple Teeth
When you have a mouth full of healthy teeth embedded in your jaw bone, you naturally stimulate bone growth through daily activities such as eating and chewing. However, when you are missing a tooth and do not replace it in a time-efficient manner, the jaw bone begins to decrease in size and strength in the area that previously anchored the tooth root. While this lack of stimulation may not appear to be a problem at first, the loss of jaw bone height and width can have a dramatic impact on the health of your mouth.
There are many reasons that you may be missing a tooth, such as a facial trauma incident that has knocked out the tooth or fractured the jaw. The consequences of tooth and jaw bone loss include but are not limited to:
- Misalignment, drifting, loosening, and loss of the remaining healthy teeth
- Collapsed facial profile
- Limited lip support
- Skin wrinkling around the mouth
- Distortion of other facial features
- Jaw (temporomandibular joint – TMJ) pain, facial pain, and headaches
- Difficulty speaking and communicating
- Inadequate nutrition as a result of the inability to chew properly and painlessly
- Sinus expansion
The rate of deterioration varies greatly among individuals, making it difficult to determine the amount of jaw bone loss an individual has suffered without proper examination by a qualified oral and maxillofacial surgeon. In general, jaw bone resorption usually begins to take place immediately following the loss or removal of a tooth and continues to worsen as time goes on.
You Suffer from Severe Periodontal Disease
Periodontal disease is one of the most common infections which affects the teeth, gum tissues, and jaw bone. There are two major types of periodontal disease: gingivitis and periodontitis. Gingivitis is primarily caused by dental plaque – the bacteria and food particles that accumulate in your mouth on a regular basis. If the teeth aren’t properly cleaned with routine hygiene efforts, the bacteria in the plaque can create swelling, inflammation, the formation of pockets in the gums (which are difficult to clean and begin to house more bacteria), and the formation of tartar (hardened plaque). If gingivitis is not treated properly, it can progress to a more severe infection – periodontitis – which causes the supporting gum tissue and bone holding the teeth in place to deteriorate and leads to tooth loosening and, ultimately, tooth loss.
You Have Unanchored Dentures or Bridgework
Unlike dental implants, unanchored dentures and bridgework do not replace the missing tooth root and contribute to jaw bone deterioration. Unanchored dentures are placed on top of the gum line and lack the ability to provide direct stimulation to the jaw bone. The imminent bone loss can lead to loosening of the denture, problems speaking and eating, and the need for a stronger adhesive or even a full new set. Bridgework is attached to two healthy teeth in the mouth which do stimulate growth; however, the area over which the bridge spans cannot properly stimulate the underlying jaw bone. A bone grafting procedure can halt and correct the jaw bone damage caused by these prosthetic options.
You Have a Jaw Bone Infection or Tumor
If you develop a jaw bone infection, such as osteomyelitis, or discover a tumor in your jaw, immediate treatment of the condition is advised to avoid inflammation, a reduction of blood supply to the bone, or spreading of the tumor to other areas of the jaw. You may need to have a portion of the jaw bone removed to mitigate the spread of the infection or tumor growth. A bone graft can be used to reconstruct and restore function to the jaw and allow for future bone growth. If the infection spreads or the tumor is malignant, additional treatment with antibiotics or the removal of soft tissue may also be required.
You Have a Genetic Defect or Sinus Deficiency
It is not uncommon for individuals to need a bone grafting procedure as a result of a birth defect. Conditions characterized by missing bone in the facial bones, jaw, or skull can be treated with this technique to replace the missing bone and stimulate healthy bone growth following the procedure. This can also be used to treat individuals who develop a sinus deficiency in the upper jaw that can occur following molar removal. As the sinuses become enlarged, the height of the jaw bone decreases, and a bone grafting procedure may be necessary to replace the missing tooth with a dental implant.
Where Does My Bone Graft Come From?
There are various bone grafting techniques that can be used to restore jaw function, and the type of bone used will depend on the specific needs of each patient. At Indianapolis Oral Surgery & Dental Implant Center, we can either obtain bone from a tissue bank for your procedure or use your own bone. If your own bone is utilized, it may be taken from the skull, jaw, hip, or tibia (below the knee), depending on the amount of bone needed for the graft. Additionally, Dr. Falender may utilize special membranes that dissolve under the gum tissue to protect the graft and stimulate healing and bone growth.
Types of Bone Grafts
- Autogenous Bone Grafts: Also known as autografts, these are made from your own bone and have the advantage of containing living cellular elements that enhance bone growth. Autogenous bone grafts require a procedure to harvest the bone prior to the graft procedure.
- Allogenic Bone: Also known as allograft, this graft is bone harvested from a cadaver, then processed using a freeze-dry method to extract the water via a vacuum. Because this bone cannot produce new bone on its own, it creates a framework for natural bone growth in the jaw.
- Xenogenic Bone: This is harvested from non-living bone of another species, usually a cow, and then processed at very high temperatures to avoid the potential for immune rejection and contamination. Like allogenic grafts, xenogenic grafts serve as a framework for bone from the surrounding area to grow and fill the void.
- Demineralized Bone Matrix (DBM)/Demineralized Freeze-Dried Bone Allograft (DFDBA): This product is processed allograft bone, containing collagen, proteins, and growth factors that are extracted from the allograft bone. It is available in the form of powder, putty, chips, or as a gel that can be injected through a syringe.
- Graft Composites: Graft composites consist of other bone graft materials and growth factors to achieve the benefits of a variety of substances. Some combinations may include collagen/ceramic composite, which closely resembles the composition of natural bone, DBM combined with bone marrow cells, which aid in the growth of new bone, or a collagen/ceramic/autograft composite.
- Bone Morphogenetic Proteins: Bone morphogenetic proteins (BMPs) are proteins naturally produced in the body that promote and regulate bone formation and healing. Synthetic materials also have the advantage of not requiring a second procedure to harvest bone, reducing risk and pain.
If you are in need of a bone grafting procedure, Dr. Falender will complete a thorough oral consultation and x-ray evaluation of your gums, teeth, and jaws. He will discuss your options for jaw bone repair so that you are fully informed on which bone grafting technique will provide you the optimal outcome that you desire. Each bone grafting option has its own risks and benefits, and we will work closely with you to develop a plan for jaw bone repair that will restore both function and aesthetics to the mouth.
Sinus Lift
How Do My Sinuses Affect My Oral Health?
It is not uncommon for patients to be unaware of the connection between the size and shape of their sinuses and the overall health of their mouth. After all, aren’t those two different facial structures? While the sinuses and the mouth are used for different purposes, they must work together to maintain healthy upper jaw bone growth, which can keep tooth roots secure.
The sinuses with the biggest impact on oral health are the maxillary sinuses, which are located behind your cheeks. These empty, air-filled spaces reside just above the upper teeth in the back of the mouth. Because the wall separating these two spaces is naturally fairly thin, it is not uncommon for some people to have their tooth roots extend up into the sinus. However, when patients lose teeth, and bone deterioration occurs, this thin membrane does not have the strength necessary to support prosthetic solutions, such as dental implant placement.
What Is a Sinus Lift?
At Indianapolis Oral Surgery & Dental Implant Center, our skilled team and surgeon, Dr. Lawrence G. Falender, offer the sinus lift procedure to increase the height and width of the bone available in the maxillary sinus. This is one of the most common treatments offered to patients who are missing teeth in the upper jaw and interested in restoring them with dental implant placement. The sinus lift procedure aims to both increase the amount of bone available for the implants to be placed as well as stimulate continuous future growth of the bone to avoid the need for additional future treatment.
If you are exploring options for tooth replacement or just looking to improve the long-term health of your remaining teeth and jaw bone, a sinus lift may be a great choice for you.
You may be a candidate for a sinus lift if:
- You have one or more missing teeth in the back of your jaw
- The bone in the back of your jaw is extremely thin
- You are missing teeth due to a birth defect or condition
- You are interested in tooth replacement with dental implants and need adequate support for the prosthesis
What Happens During the Sinus Lift Procedure?
During your initial consultation, Dr. Falender will perform a thorough oral examination and x-ray evaluation of your jaws and remaining teeth. He will develop a plan for sinus lifting that you feel comfortable with and present you with your options for sedation during the procedure. A sinus augmentation is usually performed under local anesthesia; however, some patients may request oral or intravenous sedative medication as well.
In the most common sinus augmentation procedure, a small incision is made in the premolar or molar region to expose the jaw bone. A small opening is cut into the bone, and the membrane lining the sinus is pushed upward. The underlying space is filled with bone grafting material, usually from your own body, but sometimes synthetic materials that can imitate bone formation are used. After the bone is implanted, the incision is sutured, and following several months of healing, the bone fuses with the patient’s jaw, and dental implants can be inserted and stabilized in this new sinus bone.
If enough bone between the upper jaw ridge and the bottom of the sinus is available to stabilize the implant well, sinus augmentations and implant placement can sometimes be performed as a single procedure. If not enough bone is available, the sinus augmentation will have to be performed first, then the graft will have to mature for several months, depending upon the type of graft material used. Once the graft has matured, the implants can be placed.
With the sinus lift procedure, many patients who were once told that they were not candidates for dental implant placement can now receive implant restoration. If you are interested in learning your options for bone grafting, including the sinus lift procedure, we welcome you to contact our office in Indianapolis, IN, for an initial consultation with Dr. Falender.
Ridge Augmentation
What Is a Ridge Augmentation?
The alveolar ridge bone is the bone that surrounds and supports the teeth. When a tooth is lost or removed, the empty socket in the ridge naturally heals with new tissue and bone. However, if the bone surrounding the socket breaks, healing cannot occur, and the bone begins to deteriorate or become less dense as a result.
If this occurs, a special type of bone grafting technique called ridge augmentation, or ridge expansion, can be used to restore the deteriorating bone. Ridge augmentation is different from many other bone grafting techniques because it recreates the natural contour of the gums and jaw providing a very aesthetically pleasing outcome. It also strengthens and supports the affected bone which can mitigate the possible negative consequences that resorption can have on the surrounding healthy teeth and jaw bone areas, such as:
- Tooth loosening
- Tooth loss
- Misalignment of the teeth
- Distortion of facial features and overall aesthetics
Rebuilding the original height and width of the alveolar ridge is not medically necessary but may be required for dental implant placement or aesthetic purposes. Ridge expansion is a fantastic option for patients interested in replacing missing teeth with dental implants. Dental implants require bone to support their structure, and a ridge augmentation can help rebuild this bone to accommodate the implant.
What Happens During the Ridge Augmentation Procedure?
At Indianapolis Oral Surgery & Dental Implant Center, our team wants to provide you with the most comprehensive and efficient care possible. If you elect to undergo ridge augmentation treatment, the bone graft material will be placed during the same visit in which your tooth is removed to avoid the need for a second procedure at a later date. We understand that surgery can be a stressful experience and will do everything in our power to make you feel at ease in our office and minimize your treatment time. We offer multiple options for sedation during your procedure, including local anesthesia, nitrous oxide or “laughing gas,” or IV sedation. Dr. Falender will review your options for sedation prior to the treatment and allow you to choose the option you feel most comfortable with.
During the treatment, the bone graft material is placed directly into the tooth socket. If necessary, the ridge of the jaw may be split to make room for additional grafting material. Once the graft has been placed, Dr. Falender will carefully replace the gum tissue and secure it to the gums with sutures. He may also utilize a space-maintaining product over the top of the graft to help restore the height and width of the space created by the tooth and bone loss, and into which new bone should grow.
Socket Preservation
How Does Tooth Removal Affect My Jaw Health?
It is sometimes necessary to remove a tooth or multiple teeth due to pain, infection, bone loss, or fracture of the tooth. After a tooth is extracted, the bone that holds the tooth in place, called the socket, is placed at a greater risk for damage or deterioration. When the bone in the jaw does not receive adequate stimulation, it begins to decrease in height and width, which can dramatically affect the health of the rest of the mouth. This can make it extremely difficult for your oral surgeon and dentist to perform tooth replacement procedures such as the placement of dental implants, bridges, or dentures.
What Is Socket Preservation?
Oral and maxillofacial surgeons can perform a treatment called socket preservation to mitigate jaw bone damage that can occur following tooth extractions. Socket preservation can be performed in the same surgical procedure that the tooth is removed. When the tooth has been removed from the socket, Dr. Falender will fill the socket with your own bone or a bone substitute material. He may decide to place an artificial membrane or tissue-stimulating proteins, such as platelet-rich plasma, above the graft to increase the speed of your healing. He then sutures the gums to protect the surgical site during recovery.
Patients who undergo socket preservation enjoy a variety of benefits, including:
- Elimination of shrinkage or collapse of the surrounding gums and tissues
- Stimulation of natural bone growth
- Decrease in jaw bone deterioration
- A strong foundation for implant placement
If you are in need of a tooth extraction, please inquire about socket preservation to ensure the long-term health of your teeth, gums, and jaw bone. At Indianapolis Oral Surgery & Dental Implant Center, we are happy to assist you in restoring your smile’s appearance and increasing your chances for successful dental implants for years to come.
To learn more about how we can help improve your smile, please request an appointment now.
SCHEDULE A CONSULTATION
Please contact our office by either filling out the form below or by calling us at 317-900-4535
Indianapolis Oral Surgery & Dental Implant Center





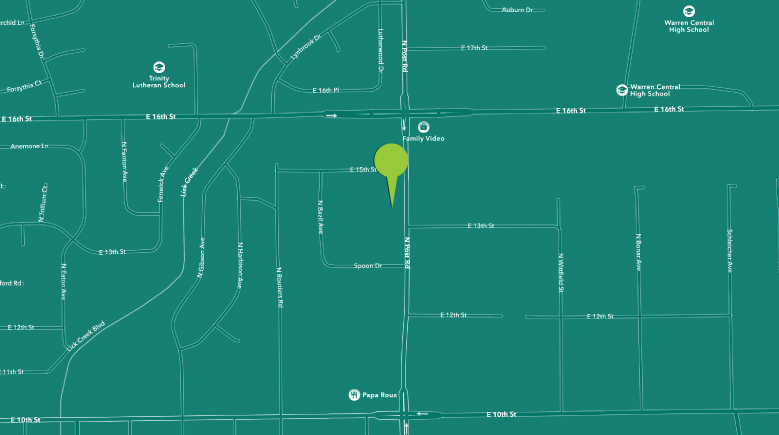
INDIANAPOLIS
Indianapolis Oral Surgery & Dental Implant Center
1320 N. Post Rd
Indianapolis, IN 46219
Main: 317-900-4535
Hours:
Se habla Español
SOCIAL